Providing culturally safe end of life care for Aboriginal and Torres Strait Islander children and young people
Wednesday, March 06, 2024
Culturally safe care for Aboriginal and Torres Strait Islander communities is an ongoing critical need in healthcare and especially so when it involves children and young people living with a life-limiting illness.
At the heart of providing culturally safe care is creating a space to hold challenging end-of-life discussions so that care can be planned in a way that honours the child and their loved ones’ choices, beliefs, and cultural needs. “The cultural and spiritual needs are so important to consider when delivering palliative care to Aboriginal and Torres Strait Islander children, young people and their families,” says Tanya Quinn, a proud Gamilaraay woman and an Aboriginal Health Worker in paediatric palliative care and chronic and complex needs at the Sydney Children’s Hospital Network.
“The connection to Country, connection to spirit, connection to community is integral in our culture,” Ms Quinn says.
“It is also critical to acknowledge the impacts of transgenerational trauma. Our mob has gone through so much trauma over hundreds of years that continues to be felt and passed through the generations.”
Sensitive communication is an important component in planning ahead. But how do we bring that to practice? The newly launched ‘Working Out What’s Right For Your Child’ discussion starter cards and the ‘Yarning Companion’ facilitator guide have been designed to support healthcare professionals start a conversation with Aboriginal and Torres Strait Islander families about end-of-life preferences for their child, or young person.
“These resources were inspired by and adapted from a more adult-focused series of discussion starters developed in 2017,” says Camilla Rowland, Chief Executive Officer, Palliative Care Australia (PCA). “In 2022, as part of the Paediatric Palliative Care National Action Plan Project, a group of health professionals from across Australia identified the need for a similar resource tailored to the specific needs that arise in the paediatric and adolescent, young adult context.”
With funding from the Australian Government Department of Health and Aged Care, a working group, which included paediatric and palliative care Aboriginal Health Practitioners, Aboriginal Health Workers, and Aboriginal Liaison Officers from urban and remote settings, came together to pursue the project.
Both the discussion starter cards and the facilitators’ guide complement each other. The cards feature specifically crafted statements that initiate respectful conversations and have been designed to be less intimidating than answering direct questions. Families and communities can select the cards that are most important to them, giving them more control in the healthcare conversation. The Yarning Companion, on the other hand, consists of guidelines that support health care providers to sensitively create space for these conversations.
Planning care for the time ahead, honours the preciousness of a child’s life highlighting to them that people and community around them, are there to support, love, and create moments of joy and connection. Importantly this process also invites the important cultural needs and rituals unique to this family or community to be known, respected and fulfilled.
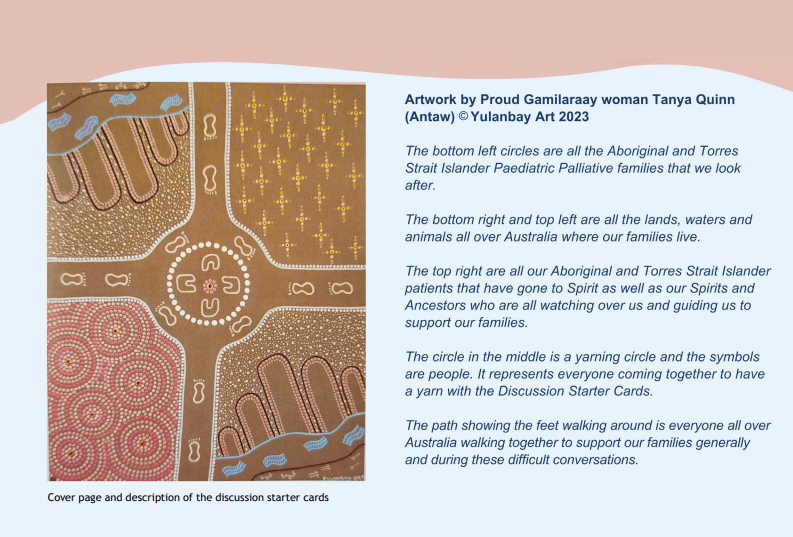
A beautiful representation of this is the artwork created by Ms Quinn for the cover of the Yarning Companion and the front side of the discussion cards. “The circle in the middle is a yarning circle…it represents everyone coming together to have a yarn with the discussion starter cards. The path
showing the feet walking around is everyone all over Australia walking together to support our families generally and during these difficult conversations.”
While these resources are a step in the right direction, it cannot replace empathetic, sensitive, human connection. It is important that health care teams build trust and rapport from the very start in conjunction with their Aboriginal health workers. “Sit down and have a yarn, have a yarn and get to know them [the child or young person] and their family, make that conscious effort, it’s really not that difficult. Let’s not assume anything. Communication can make everything so much easier,” Ms Quinn says.
The ‘Working Out What’s Right For Your Child’ discussion starter cards and the ‘Yarning Companion’ facilitator guide are available on the Paediatric Palliative Care website.
“These resources are a great asset to anyone working in paediatric palliative care. The support and skills it’ll provide health professionals will be invaluable in initiating those difficult conversations in a sensitive way and providing care that is culturally safe,” Ms Rowland says. “I look forward to seeing these resources empowering health professionals, volunteers, and Aboriginal and Torres Strait Islander children and communities.”
The Paediatric Palliative Care National Action Plan Project is a collaboration between Palliative Care Australia and Paediatric Palliative Care Australia and New Zealand and is funded by the Australian Government Department of Health and Aged Care.
This story was first published in the February issue of The Health Advocate magazine by the Australian Healthcare and Hospitals Association (ahha).
Select where you would like to share this article
Close WindowWe recognise and acknowledge those who are working through Sorry Business, Sad News, grief and bereavement and offer our condolences and support.
Aboriginal and Torres Strait Islander peoples are advised that this website may contain images, videos and voices of people who have passed on. Some of the content and topics covered might also cause distress. You are welcome here, and we want you to feel safe and take care.
If you find that you need support please reach out to 13YARN on 13 92 76, Grief Australia, Grief Line on 1300 845 745, or Lifeline on 13 11 14.
Palliative Care Australia is located in Canberra. We acknowledge the traditional custodians of the surrounding land and waters, the Ngunnawal and Ngambri Peoples and pay our respects to Elders past and present. We extend that same respect and acknowledge the continuing cultures and contribution of Aboriginal and Torres Strait Islander Peoples across Australia.
Close